Murray J. McAllister, PsyD
Murray J. McAllister, PsyD, is a pain psychologist and consults to health systems on improving pain. He is the editor and founder of the Institute for Chronic Pain (ICP). The ICP is an educational and public policy think tank. In its mission is to lead the field in making pain management more empirically supported, the ICP provides academic quality information on chronic pain that is approachable to patients and their families.
What is rehabilitation?
People often equate rehabilitation with physical therapy. It’s something a patient does following an injury or surgery. Rehabilitation is also something that one does after a catastrophic injury or illness, such as having a stroke, a traumatic brain injury, spinal cord injury, or long-haul COVID. Still others think of rehab as a treatment for alcoholism or drug addiction. Rehabilitation can also be a form of vocational counseling. Injured workers re-learn how to go back to work in what’s called vocational rehabilitation.
It often comes as a surprise to patients that chronic pain rehabilitation programs are typically the most effective form of treatment for patients with chronic (non-cancer) pain syndromes. As a society, we tend to assume that medications, procedures and surgeries are not only effective, but are the most effective treatments for chronic pain. But, it’s not the case.
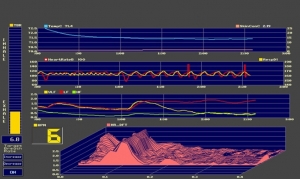
Biofeedback
What is biofeedback?
Biofeedback is a treatment used for a variety of chronic pain and other medical conditions that consists of sensors placed on the patient’s body while physiological data is viewed on a computer screen or other monitor in real time. It is considered a self-regulatory therapy because it is a tool for increasing awareness of and changing individual physiological responses to reduce symptoms or improve performance. The Association for Applied Psychophysiology and Biofeedback (AAPB), the Biofeedback Certification International Alliance (BCIA), and International Society for Neurofeedback and Research (ISNR) provide this standard definition:
Benefits of Managing Chronic Pain without Opioids
On initial reaction, it might seem absurd to talk about the benefits of self-managing chronic pain without opioid medications. "What," one might ask, "would you use to reduce pain? You wouldn't want to live the rest of your life in pain, would you?" The topic seems absurd because pain reduction reflexively seems so important. Indeed, pain reduction from the use of opioids seems so important that it trumps everything else, even problems associated with the use of opioids.
What is the Neuromatrix of Pain?
The notion of a neuromatrix of the brain is a theoretical model that explains the nature of pain, including chronic pain. Ronald Melzack, PhD, a psychologist, and one of the founding fathers of the field of pain management as we know it today, developed the theory and published it in a series of papers at the end of the last century.1, 2, 3, 4 Melzack had previously revolutionized the field of pain management in an earlier theory that he had developed and published with his physician colleague, Patrick Wall, in what is known as the gate control theory of pain.5 Few theories in modern science have spawned more empirical research than those of the gate control theory of pain and the neuromatrix of pain. Indeed, while technically theories, the field largely considers these models as accurate explanations of the nature of pain, given the great wealth of empirical evidence that now confirms them. So, what is this notion of the neuromatrix of the brain that explains the nature of pain?
Few topics in healthcare generate more passion than the use of opioid medications for chronic, non-cancer pain. Some, in the debate, lead the charge for greater access to opioids, arguing fervently that these medications are under-prescribed, while others call for more limited access, arguing that opioids are over-prescribed. The central focus for these strong feelings is typically the issue of addiction, but other issues commonly receive attention as well, such as the effectiveness of opioids and humanitarian calls to alleviate suffering.
While it appears that the Affordable Care Act (ACA) may have slowed the rate of annual increases in health insurance premiums, the overall cost of health insurance continues to rise.1, 2, 3 Employers subsequently continue to face the dilemma of either absorbing these annual cost increases and thereby reduce potential profit or passing these costs onto their employees and thereby reduce their potential take-home pay. In other words, do you face the ire of shareholders or workers?
Educational Links
Chronic Pain Rehabilitation Programs
The American Chronic Pain Association provides information on chronic pain rehabilitation programs.
A TED Talk by Tracy Jackson, MD, of Vanderbilt University, on interdisciplinary chronic pain rehabilitation programs (aka, functional restoration programs).
How to End the Stigma of Pain
Stigma is a significant and persistent problem for those with chronic pain. Stigma occurs when someone is judged for having a condition that they didn't choose to have, like chronic pain. In other words, stigma is the criticism of being bad in some way for simply having a condition that you didn't choose to have. It can also occur in relationship to how a patient with chronic pain is coping. Stigma thus arises when moral judgments occur not for wrong behavior, which might rightly get criticized, but for simply being who you are, for simply having the health condition that you have, or for how you are dealing with it.
Profit-Motive and Pain Management
One of the more common sentiments that chronic pain patients express is that that the profit-motive seems to have had too much of an influence on the recommendations that their healthcare providers have made over the years. After reflecting on all the years of chronic pain and all the years of failed treatments, many of which were tried again and again despite having failed to reduce pain at previous clinics, they conclude that the business side of healthcare has played too much of a role in their own care. They are now disappointed, angry, and distrustful of chronic pain management providers.